YOUR FITNESS BLOG
Why Might Grains Make You Feel Sick?
Introduction
Grains have emerged as a staple food in the modern day diet. For some individuals, consumption of certain grains like rice, wheat germ, rye, and barley can result in adverse health reactions including constipation, gas, or bloating. It is proposed that grains today are very different that what was cultivated before the industrial era and that the crossbreeding and hybridisation of grains contribute to the adverse health symptoms some experience. This blog post will look into the evolution of grains to understand why some people may reactively negatively to their consumption.
Didn’t We Always Eat Grains?
Fossil records of tools used to grind and cook wild cereal grains provide a reliable indication of when and where cultures around the world began to use grains in their diet [9]. Archaeology records show that regular use of grains by any hunter-gatherer group appeared approximately 12,800 – 10,300 years ago in the Levant region (modern Palestine, Israel, Syria and Jordan), among a hunter-gatherer culture know as the Natufians [9, 21]. Prior to the Epi-paleolithic (10,000 –11,000 years ago) and Neolithic periods (10,000 – 5,500 years ago), it is suggested there was little or no evidence of cereal grain consumption [8].
There is evidence to suggest the first wild, cultivated wheat was called einkorn [8, 11]. Einkorn had the simplest genetic code of all subsequent wheat. Shortly after came the wheat called emmer [8, 11].
Natufians, a late Epi-Paleolithic hunter-gatherer population, are said to have harvested wild einkorn and emmer wheat that eventually became an essential part of their diet and reduced the need for hunting and gathering [8]. Domestication of emmer and einkorn wheat by Natufian descendants marked a fundamental shift to cultivating grains and the beginning of agriculture [11, 8].
Original einkorn and emmer are shown to be very different to our twenty-first century wheat. Einkorn and Emmer wheat were “hulled,” meaning the seeds clung tightly to the stem [11]. Compare this to the modern day “naked” form of wheat where the seeds easily separate from the stem. More importantly, modern wheat is crossbred and hybridized tens of thousands of times over with different wheat’s and grasses, which dramatically change the genetic makeup of wheat [11]. The mass yielding of modern wheat with its dramatic modifications and variations in enzyme, protein and gluten content have ultimately come at the cost of human health [11].
The industrial revolution (1760 – 1850) marked the advent of mechanized steel roller mills and automated sifting devices making grains available for mass production [8]. Prior to the industrial revolution, cereal grains were ground using stone milling tools, soaked, sprouted, fermented and roasted [1, 18]. They contained the entire contents of the cereal grain, including the germ, bran, and endosperm [18]. Today, the nutritional elements of grains are very different as the germ and bran are removed in the milling process, yielding flour composed of mainly endosperm [8].
Are There Potential Health Hazards With Grains?
Grains are the seeds of plants. They are the reproductive material of each plant and in accordance with evolutionary strategy, plants, like animals, have mechanisms for protecting themselves [18]. As protective mechanisms to defend themselves against predators, some plants produce toxins that damage the gut. It is proposed that these toxins bind to minerals in our body, possibly making them unavailable for the body to use and prevent the digestion and absorption of essential nutrients [18].
Gluten
One of these toxins found in plants is suggested to be gluten. Gluten is a protein found most abundantly (80%) in wheat, but also present in:
- Wheat germ
- Rice (brown, white, wild)
- Rye
- Barley
- Bulgur
- Couscous
- Farina
- Graham flour
- Kamut Matzo
- Semolina
- Spelt
- Triticale
Although other non-grains such as amaranth, buckwheat, millet, quinoa, sorghum, teff, oats and corn do not naturally contain gluten, they are frequently contaminated with gluten as they are processed at mills that also handle wheat [18]. A 2014 article by Lee and colleagues showed that of the 78 randomly selected food samples labeled “gluten free,” 16 (20.5%) contained gluten levels equal to or above the defined gluten-free level (20 mg/kg) [19]. In particular, five of eight breakfast cereal samples showed gluten contents higher than 20 mg/kg [19].
In a previous article we discussed the potential immune responses to gluten proteins. In this article we highlight celiac disease, an autoimmune condition (where the body attacks its own cells and tissues) triggered by gluten and may lead to inflammation and damage to the tissues in the small intestine [18]. Also, we now know it is possible to be intolerant to gluten, independent of celiac disease, with a condition known as non-celiac gluten sensitivity (NCGS), a disorder that carries a multitude of symptoms within and outside the digestive tract [11].
In the last decade, NCGS has received growing attention as patients have reported more severe nonspecific symptoms with gluten intake than seen with classic celiac disease [2, 12, 20]. Specifically, non-celiac gluten sensitivity has been linked to allergies [20]. In 2011, Massari and colleagues biopsied 262 patients with both classical allergy (asthma, dermatitis) and gastrointestinal (stomach pain, diarrhoea, weight loss) symptoms [20]. In approximately 30% of allergic patients, the authors found lesions in the small intestines and villous atrophy (erosion of the tiny finger-like projections in the intestines that help to absorb nutrients) [20]. Interestingly, these authors observed a significant improvement in health state of the positive patients when they followed a gluten-free diet [20].
Also, gluten was found to worsen symptoms in NCGS individuals with irritable bowel Syndrome (IBS) [2]. A 2011 double-blinded, randomised controlled trial, randomly allocated 34 people to either a gluten or placebo group, where subjects received two bread slices and one muffin per day for 6-weeks [2]. Of the 19 patients in the gluten group, 13 reported worsening of their symptoms (pain, bloating, tiredness, stool inconsistency) within 1-week compared to 6 of the 15 patients in the placebo group [2].
A link between gluten and autism, schizophrenia and attention deficit/hyperactivity disorder has further been suggested [11, 12]. Increased intestinal permeability, referred to as “leaky gut syndrome” have been suggested in autism spectrum disorder (ASD) as part of the chain of events that allow peptides to cross the intestinal barrier, enter the bloodstream, then cross the blood-brain barrier (layer of cells separating the bloodstream from the brain) [12]. It has been suggested that wheat polypeptides bind to the brain’s morphine like receptor, the very same receptor to which opiate drugs bind, resulting in an excess of opioids thought to lead to ASD behaviors [11, 12]. A high percentage of abnormal intestinal permeability (IPT) was found among patients with autism compared with normal individuals [12].
Gliadins
Gliadin is protein found in wheat gluten. The group of gliadin proteins are those that are said to most strongly trigger the immune response in individuals with celiac disease [11]. Specifically, it has been suggested that gliadin increases intestinal permeability (“leaky gut”) by way of an intestinal peptide called zonulin [14]. A study by Drago and colleagues in 2006 showed that gliadin released zonulin causing disruption in the tight barrier that prevents toxins from entering the bloodstream leading to increased intestinal permeability [14]. High zonulin levels (together with increased intestinal permeability) have been observed in autoimmune and inflammatory diseases like celiac disease, multiple sclerosis, asthma and inflammatory bowel disease [11, 14].
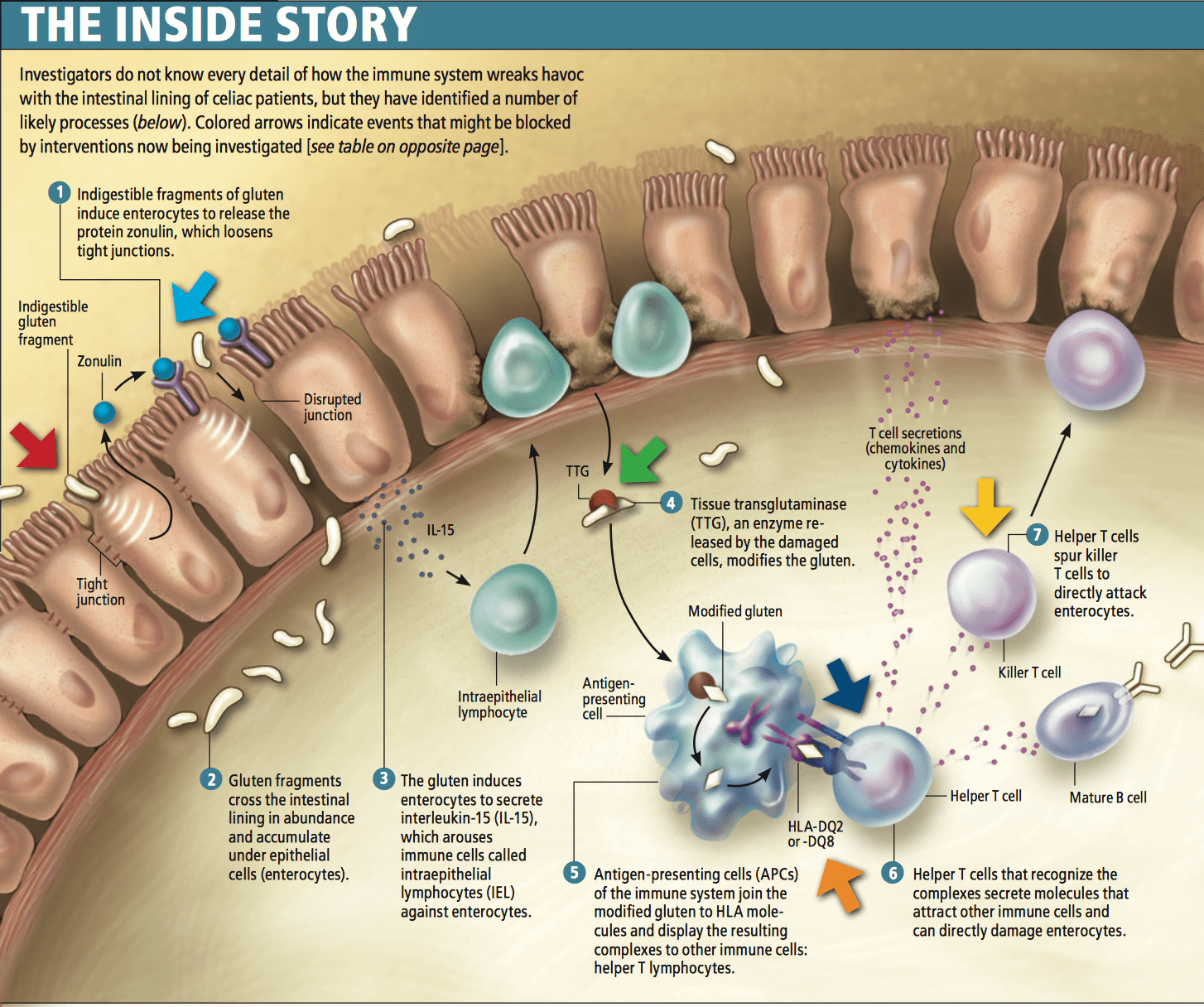 [Image: Fasano, A. 2009. Scientific America]
[Image: Fasano, A. 2009. Scientific America]
Gliadin may therefore induce the production of pro-inflammatory cytokines (messenger cells) in celiac or non-celiac individuals [2]. The activation of these pro-inflammatory cytokines may lead to low-grade inflammation in the body, said to be the root cause of all modern diseases like cardiovascular disease, obesity, and autoimmune diseases [2, 18].
Lectins
Similar to gliadins, lectins are proteins found in plants and are said to have evolved as a toxic defence mechanism to ward off predators [2, 17]. Plant lectins are usually at highest concentrations in plant parts because they are essential for plant reproduction [17]. Just like gliadins, most plant lectins are resistant to heat and digestive enzymes and are said to be capable of binding and damaging several tissues and organs in the body [2]. Lectin activity has been demonstrated in wheat, rye, barley, oats, corn, rice and most abundantly in wheat germ like in unprocessed muesli and many breakfast cereals [23].
A type of lectin known as wheat germ agglutinin (WGA), present in wheat seed in both the germ and the gluten part of endosperm, has been more extensively studied because of its potentially health damaging effects. Each grain contains about one microgram of WGA and its function is to protect the plant against insects and fungi [17]. It is suggested that WGA may cause an inflammatory response by way of stimulating several pro-inflammatory cytokines in the body [13]. Higher WGA antibodies have been found in individuals with celiac disease compared to those with other intestinal disorders indicating a greater immune defence response among celiac sufferers [13].
After digesting foods with WGA like breakfast cereals, it is suggested that WGA is capable of crossing the intestinal barrier into the blood circulation, thereby allowing microbial and dietary toxins to interact with cells of the immune system [13]. The result may be enhanced symptoms within (diarrhoea, constipation, gas, bloating) and outside (headaches, lethargy) the gastrointestinal system in both celiac and non-celiac gluten sensitive individuals.
Research shows that WGA may also be toxic to the brain. Though a process called “absorptive endocytosis,” WGA is able to travel among the tissues of the brain passing through the blood brain barrier (BBB) pulling bound substances with it disrupting neuronal membranes [13]. This disruption of neuronal membranes may be linked to neurodegenerative disorders like Parkinson’s, Alzheimer’s and Huntington’s disease.
Ingestion of WGA has been also been found to have an insulin-like effect, which may contribute to weight gain [25]. Specifically, lectin has been linked to obesity and “leptin resistance.” In a previous article, we discussed leptin (not lectin, try not to confuse the two!) and identified leptin as a hormone made by adipose (fat) cells in the body that functions as our satiating hormone signalling to the brain to inhibit food intake [17, 23]. Leptin resistance is when this hormone is unable to function properly and the body wants to excessively eat because it thinks it’s starving [23]. Lectins ingested through grains can bind to the leptin receptor in the brain (hypothalamus) and negatively affect its function [17, 23].
Phytates
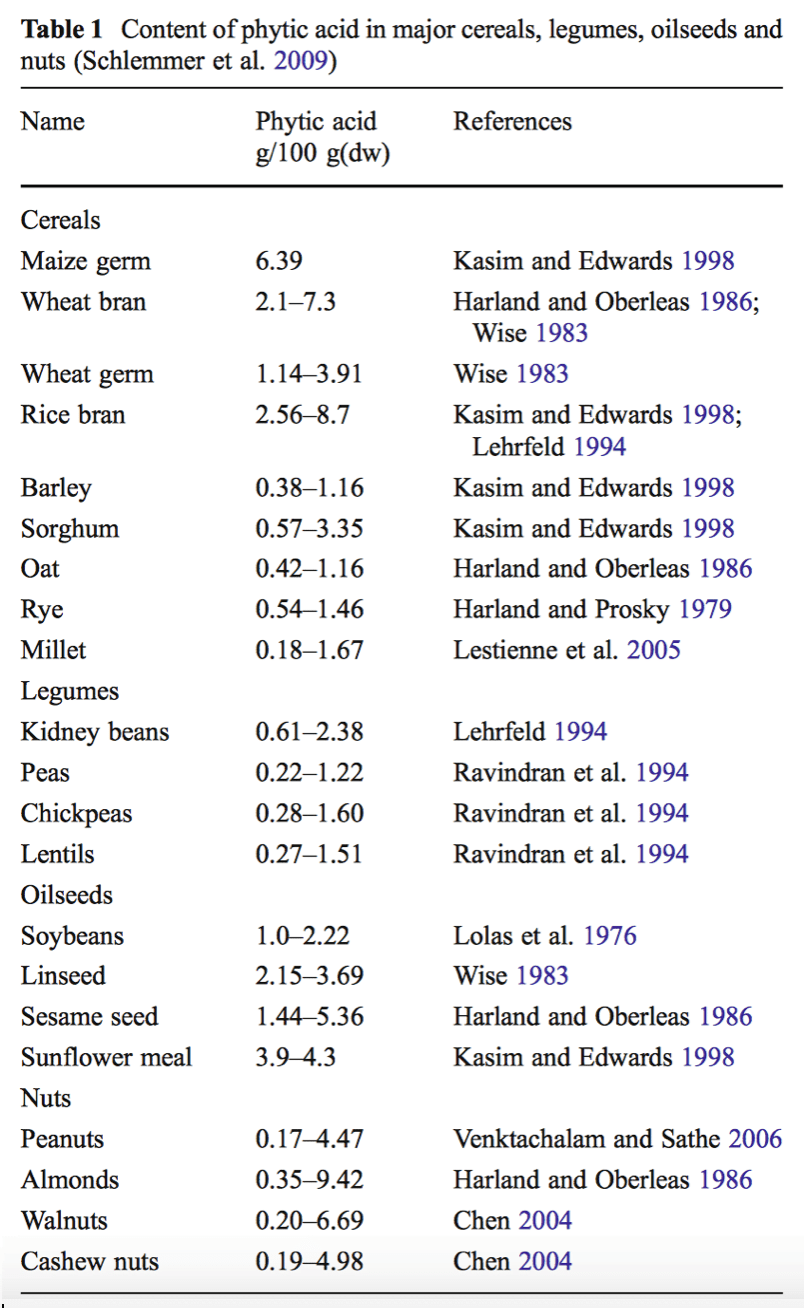
Phytates or phytic acid are compounds typically found in the outer layers of cereal grains and in the endosperm of legumes and seed oils [1, 3]. Phytates are the major storage form of phosphorus in all grains, nuts, seeds and beans and function as an essential energy source for the sprouting seed [1, 3]. Often labelled as “anti-nutrients,” the phytates in grains are proposed to have an inhibiting effect potentially binding onto important minerals and trace elements like iron, zinc, calcium and manganese, the result of which may be malabsorption of nutrients in phytate containing grains and possible mineral deficiency [1, 3].
A 2004 study by Bohn and colleagues examined the effect of phytic acid on magnesium absorption among 20 (10 men and 10 women) healthy subjects [3]. The authors added phytic acid to 200g of white-wheat bread and whole-meal wheat bread and subject faecal samples were collected to test mineral absorption [3]. Magnesium absorption was shown to be approximately 60% lower when phytic acid was added to white-wheat bread and 25% lower when added at an amount similar to that in brown bread [3].
Phytic acid has also been shown to bind to iron in the body. A 1992 study by Brune and collegues showed that iron content were reduced in five different types of rye or wheat bread compared to iron absorption from white bread [4]. The authors noted their findings “clearly indicate that the inhibition of iron absorption by wheat and rye bran could be ascribed to its content of phytate” [4].
There are several methods that traditional cultures like the Natufians would have used, which would remove or dramatically reduce the phytic acid in grains, therefore enhancing nutrient absorption.
- Milling and soaking milling
- Fermenting
- Germinating
However, important to note that more recent research suggests that phytic acid may actually exhibit protective health effects as an anti-cancer and anti-inflammatory compound [1, 22]. Ironically, it is suggested that phytic acid may act as an antioxidant by way of its iron and copper binding effects [1]. A number of studies have suggested the potential anti-cancer effects of phytic acid [1, 15, 22]. Studies by Shamsuddin et al. (2002) and Catherine and colleagues (2007) suggest phytic acid may lower blood glucose response by reducing the rate of starch digestion and slowing the gastric emptying, therefore exerting health benefits for diabetes patients [22, 7]. It is clear more research in this area is needed to clarify the potential health damaging or preserving effects of phytic acid.
Summary
It is suggested that dietary and lifestyle changes that began with the agricultural era approximately 11,000 years ago were too recent on an evolutionary time scale for the human genome to adapt [8, 5]. Prior to agricultural revolution and the domestication of animals, human diet would have been limited to minimally processed, wild plant and animal foods [5]. With the advent of agriculture and most certainly the industrial era, grains have accelerated to become a staple in the human diet. As processed foods have become ubiquitous in the modern day diet (eg, cookies, cakes, bakery foods, breakfast cereals, bagels, rolls, muffins, crackers, chips, and other snack foods), it is suggested these foods are largely to blame for the global increase of non-communicable disease like obesity and cardiovascular disease.
It is also theorised that toxins inherent in plants have the potential to cause substantial damage, altering the microorganism in the digestive system, increasing intestinal permeability and leading to low-grade inflammation [5]. If negative reactions are identified with grain consumption, substituting grains with alternatives like coconut and soaking or sprouting nuts and seeds to break down phytic acid has been advocated as a method to potentially reduce toxicity as well as the dietary integration of non-grains like quinoa and buckwheat.
For more information on our personal training services please click here to read more.
References:
1. Admassu, S. 2009. Potential Health Benefits and Problems Associated with Phytochemicals in Food Legumes. East African Journal of Sciences. Vol. 3, No. 2, pp.116-133.
2. Biesiekierski, J. R., et al. 2011. Gluten Causes Gastrointestinal Symptoms in Subjects without Celiac Disease: A Double-Blinded, Randomised, Placebo-Controlled Trial. The American Journal of Gastroenterology. March. Vol. 106, No. 3, pp. 508-514.
3. Bohn et al. 2004. Phytic acid added to white-wheat bread inhibits fractional apparent magnesium absorption in humans. American Journal of Clinical Nutrition. March. Vol. 79, No. 3, Pp. 418-423.
4. Brune, M. et al. 1992. Iron Absorption from Bread in Humans: Inhibiting Effects of Cereal Fiber, Phytate and Inositol Phosphates with Different Numbers of Phosphate Groups. The Journal of Nutrition. March. Vol. 122, No. 3, pp.442-449.
5. Carrera-Bastos et al. 2011. The Western Diet and Lifestyle and Diseases of Civilization. Research Reports in Clinical Cardiology. March. Vol. 2. Pp.15-35.
6. Catassi, C. et al. 2013. Non-Celiac Gluten Sensitivity: The New Frontier of Gluten Related Disorders. Nutrients. October. Vol.5, No.10, pp. 3839-3853.
7. Catherine, C. N. 2007. Cranberry and its phytochemicals: A review of in vitro anti-cancer studies. Supplement: International research conference on food, nutrition, and cancer. Journal of Nutrition. January. Vol. 137, No. 1, pp. 186S-193S.
8. Cordain, L. et al. 2005. Origins and evolution of the Western diet: health implications for the 21st century. American Journal of Clinical Nutrition. February. Vol. 81, No.2, pp.341-354.
9. Cordain, L. 1999. Cereal Grains: Humanity’s Double-Edged Sword. World Review of Nutrition and Dietetics. Vol. 84, pp. 19 –73.
10. C3 Collaborating for Health. 2011. Non-communicable diseases in the UK: NCDs Worldwide [online]. London: C3 Collaborating for Health. [viewed 30 December 2015]. Available from: http://www.c3health.org/wp-content/uploads/2009/09/NCDs-briefing-paper-20111010.pdf.
11. Davis, W. 2011. Wheat Belly. Canada: Collins.
12. de Margistris, L., et al. 2010. Alterations of the Intestinal Barrier in Patients With Autism Spectrum Disorders and in Their First-degree Relatives. Journal of Pediatric and Gastroenterology. October. Vol. 51, No.4, pp.418-424.
13. de Punder, K. & Pruimboom, L. 2013. The Dietary Intake of Wheat and other Cereal Grains and Their Role in Inflammation. Nutrients. March. Vol. 5, No. 3, pp. 771-787.
14. Drago, S. et al. 2006. Gliadin, zonulin and gut permeability: Effects on celiac and non-celiac intestinal mucosa and intestinal cell lines. Scandinavian Journal of Gastroenterology. April. Vol. 41, No. 4, pp. 408-419.
15. Fournier, D.B. and Gordon, G.B. 2000. Cyclooxygenase- 2 (COX-2) and colon cancer: potential targets for chemoprevention. Journal of Cell Biochemistry. Vol. 34, pp. 97-102.
16. Geoba., 2015. The World: Life Expectancy [online]. [Viewed 30 December 2015]. Available from: http://www.geoba.se/population.php?pc=world&type=15.
17. Jonsson, T. et al. 2005. Agrarian diet and diseases of affluence – Do evolutionary novel dietary lectins cause leptin resistance? BMC Endocrine Disorders. December. Vol. 5, No. 10.
18. Kresser, C. 2013. The Paleo Code. Grains and Pseudocereals. New York: Little, Brown and Company. pp.188-190.
19. Lee et. al. 2014. Gluten Contamination in Foods Labeled as ‘‘Gluten Free’’ in the United States. Journal of Food Protection. October. Vol. 77, No. 10, pp. 1830–1833.
20. Massari, S. et al. 2011. Occurrence of Nonceliac Gluten Sensitivity in Patients with Allergic Disease. International Archives of Allergy and Immunology. February. Vol.155, No.4, pp.389-394.
21. Ofer Bar, Y. & Lieberman, D. E. 1994. The Natufian Culture in the Levant. Journal of Field Archaeology. Autumn. Vol. 21, No. 3, pp. 376-378.
22. Shamsuddin, A. M. 2002. Anti-cancer function of phytic acid. International Journal of Food Science and Technology. October. Vol. 37, No. 7, pp. 769-782.
23. Unger, R. H. 2005. Longevity, lipotoxicity and leptin: the adipocyte defense against feasting and famine. Biochimie. January. Vol. 87, No. 1, pp. 57-64.
24. World Health Organisation. 2015. Chapter 1: Burden: mortality, morbidity and risk factors [viewed 31 December 2015]. Available from: http://www.who.int/nmh/publications/ncd_report_chapter1.pdf
25. Yevdokimova, N. Y. and Yefimov, A. S. 2001. Effects of Wheat Germ Agglutinin and Concanavalin A on the Accumulation of Glycosaminoglycans in Pericellular Matrix of Human Dermal Fibroblasts. A Comparison with Insulin. Acta Biochimica Polonica. November. Vol 48, No. 2, pp. 563-572.

Did you find this content valuable?
Add yourself to our community to be notified of future content.